In the 1990s, molecular cloning techniques became standard for generating recombinant DNA, allowing researchers to insert and delete genes within an organism’s genome. This brought about a resurgence of interest in oncolytic viruses.
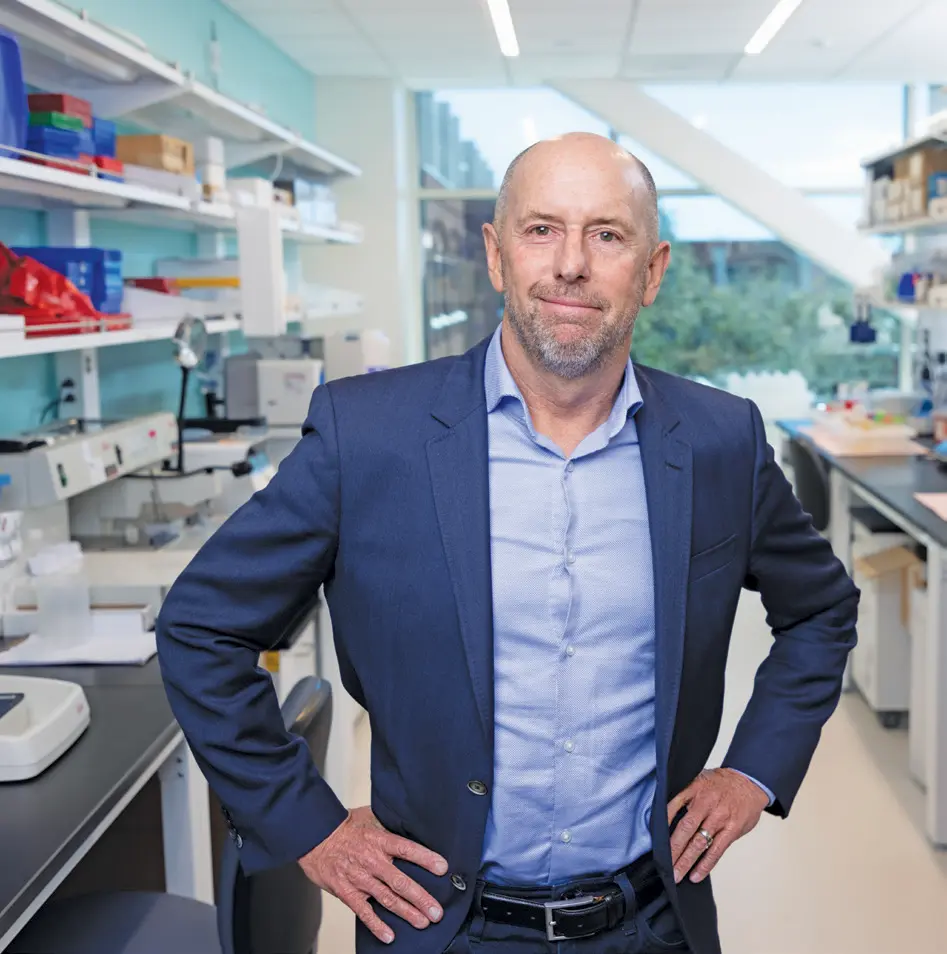
In 1994, David Kirn, now CEO and cofounder of 4D Molecular Therapeutics, completed his fellowship in medical oncology at the University of California, San Francisco, and was looking for a research project. With an interest in virology, Kirn interviewed with Onyx Pharmaceuticals, a newly founded company developing novel cancer therapies.
“They said there was this idea of using viruses against cancer,” Kirn remembered. “I’d always been torn between my love of virology, infectious disease, and oncology. So, for me, it was the perfect fit.”
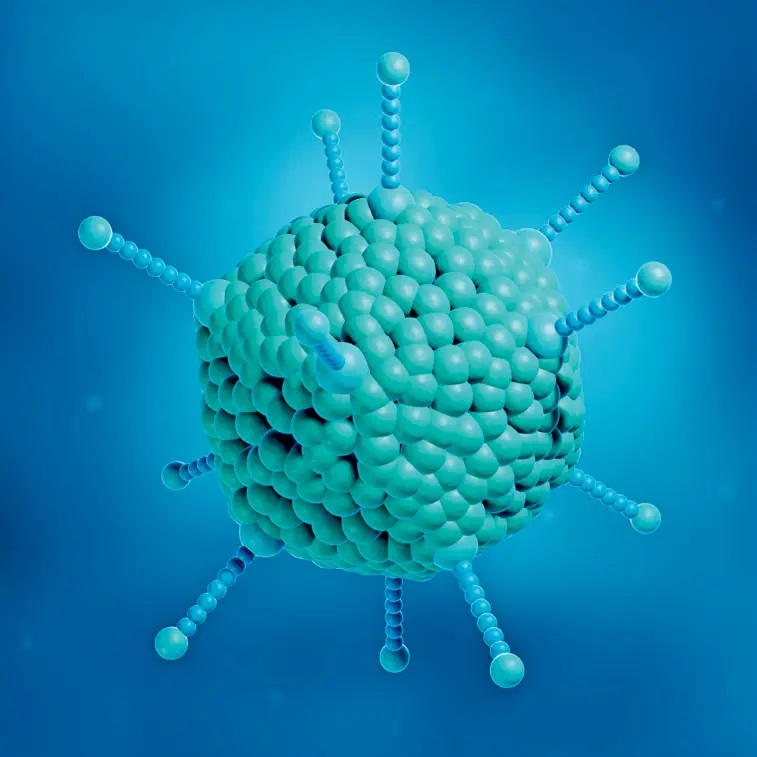
Kirn became Onyx Pharmaceuticals’ tenth employee and started working on creating new viruses that could selectively target cancer cells. “There were no engineered viruses that had been in the clinic before,” Kirn said. The only related research he found was by Robert Martuza, a neurosurgeon at Massachusetts General Hospital, who had genetically modified a herpes simplex virus by deleting the thymidine kinase gene in 1991. With this modification, the virus replicated only in rapidly dividing tumor cells and inhibited tumor growth in mice (8).
Inspired by Martuza’s study, Kirn worked with adenovirus, deleting its E1B gene to create a modified virus named ONYX-015. The E1B gene encodes a protein that binds to and inactivates the tumor suppressor p53 protein, preventing p53-mediated apoptosis and allowing viral replication in infected cells. Without the E1B gene, the ONYX-015 virus cannot inactivate p53 and cannot replicate in normal cells. However, it can replicate efficiently in p53-deficient tumor cells.
In 1997, Kirn and his team published results showing ONYX-015’s remarkable antitumor effects in mice with a substantial reduction in tumor size and complete regression in 60 percent of the tumors (9). While presenting these encouraging results, Kirn and his team were also getting ready to test ONYX-015 in human trials.